Blog

The Centers for Disease Control estimates that around 2.8 million people in the United States suffer from a traumatic brain injury (TBI) every year, and vision can be affected. Concussions are a type of TBI.
The rate of childhood TBI visits to the emergency department more than doubled between 2001 and 2009, making children more likely than any other group to go to the ER with concussion symptoms.
It was once assumed that the hallmark of a concussion was a loss of consciousness. More recent evidence, however, does not support that. In fact, the majority of people diagnosed with a concussion do not experience any loss of consciousness. The most common immediate symptoms are amnesia and confusion.
There also are multiple visual symptoms that can occur with a concussion, either initially or during the recovery phase.
Visual symptoms after a concussion include:
Blurred vision.
Difficulty reading.
Double vision.
Light sensitivity.
Headaches accompanying visual tasks.
Loss of peripheral vision.
Most people with visual complaints after a concussion have 20/20 distance visual acuity, so more specific testing of near acuity, convergence amplitudes, ocular motility, and peripheral vision must be done.
In a study done at the Minds Matter Concussion Program at the Children's Hospital of Philadelphia, patients with a concussion diagnosis underwent extensive vision testing, which assessed symptoms, visual acuity, eye alignment, near point of convergence, vergence amplitude and facility, accommodative amplitude and facility, and saccadic eye movement speed and accuracy.
A total of 72 children (mean age 14.6 years) were examined, and 49 (68%) of those
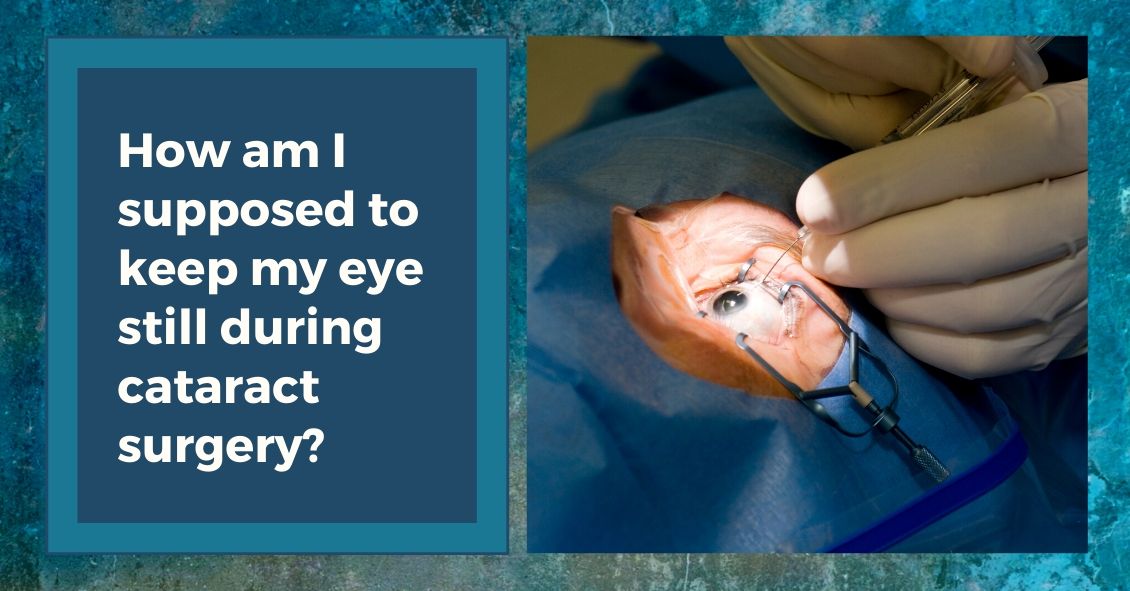
The majority of cataract surgeries performed in the U.S. are done with a local anesthetic and IV sedation.
The local anesthesia may be accomplished in one of two ways: either an injection of anesthetic around the eye or anesthetic eye drops placed on the eye, often combined with an injection of a small amount of anesthetic into the front of the eye at the very beginning of surgery.
The injection of anesthetic around the eye generally produces a deeper anesthesia for the surgery than the topical method but it also comes with increased risk. There is a very small chance of potentially serious bleeding behind the eye and a rare chance of inadvertent penetration of the back of the eye with the injection needle.
The topical anesthesia has lower risk but does not provide quite as deep of an anesthesia, although the overwhelming majority of people having cataract surgery with a topical anesthetic do not experience any significant pain during the procedure.
The other difference between the two anesthesias is with that topical anesthesia you maintain your ability to move your eye around whereas with injection anesthesia the eye muscles are temporarily paralyzed so your eye doesn’t move during the surgery. When you have topical anesthesia it is important for you to try to stare straight ahead at the light in the microscope above you. Most people accomplish this quite easily.
Along with the anesthetic to the eye, in most cataract surgeries an anesthetist will also give you some